Automating Claims Documentation for an InsurTech SaaS Company
Making insurance claim processing faster and more efficient with AI
AI development
Insurance
9 weeks
Web
About the project
Our client is a US-based Insurtech company that offers a SaaS platform for insurance brokers and claims adjusters. Their goal is to reduce the administrative burden on insurance professionals by automating claims documentation, one of the most repetitive and time-intensive tasks in the industry. They wanted their platform to automatically extract relevant data from claim documents, summarize policy details, and generate initial claim assessments based on voice notes and uploaded forms.
The client had
A working SaaS platform
Document upload and voice memo features
Limited in-house AI expertise and development bandwidth
We were responsible for
AI/NLP pipeline for document and voice input analysis
Backend/API integration with insurance databases
Frontend updates to display AI-generated summaries and claim suggestions
Project Team
Project manager
UX/UI designer
Full-stack engineer
AI engineer
QA engineer
DevOps
Conceptual flow diagram
AI-Powered claims documentation automation.
Input Sources (User Actions)
Uploaded Claim Forms, Voice Notes, Attachments and Supporting Docs
Intelligent Data Extraction
NLP + OCR, Extracts policyholder info, Pulls out claim details, Interprets audio notes
Automated Understanding & Structuring
Summarization of Policy Terms, Classification of Claim Types, Tagging Key Events & Entities
Initial Claim Assessment
Draft Claim Summary, Risk Flags / Coverage Checks, Actionable next steps for adjuster
Output
Structured Claim Document, Internal System Notes, Feedback Loop for Adjuster Input
Scope of work
To bring the solution to life, we followed a structured development process tailored to the client’s domain. Below is a breakdown of the key stages involved, from initial feasibility assessment to full system integration.
Requirements gathering and feasibility study
AI/NLP model selection and fine-tuning
Custom prompt engineering for insurance-specific language
Voice-to-text pipeline integration for recorded claim statements
Auto-generation of claim summaries and recommendations using LLMs
Integration with insurance policy and claims management systems
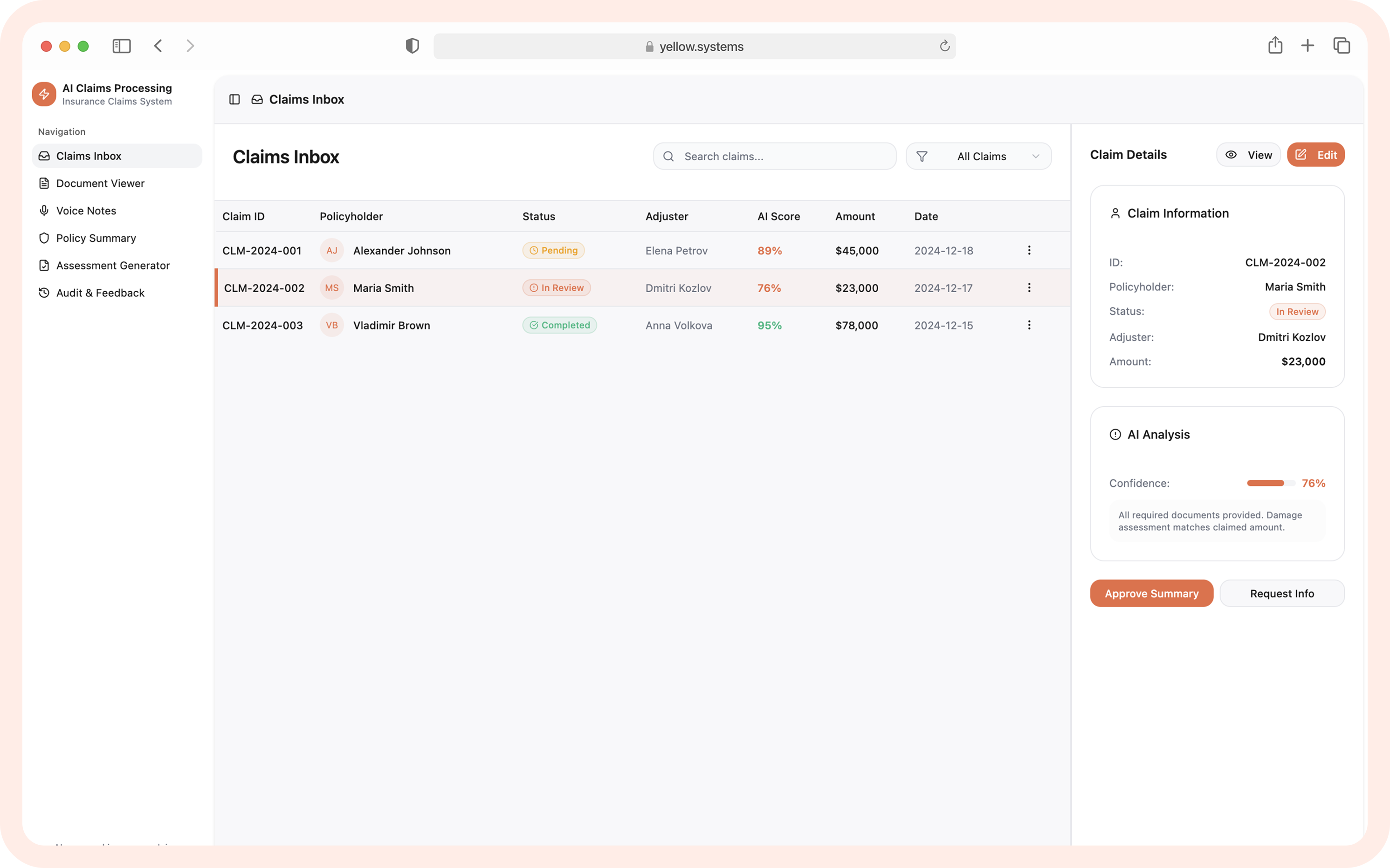
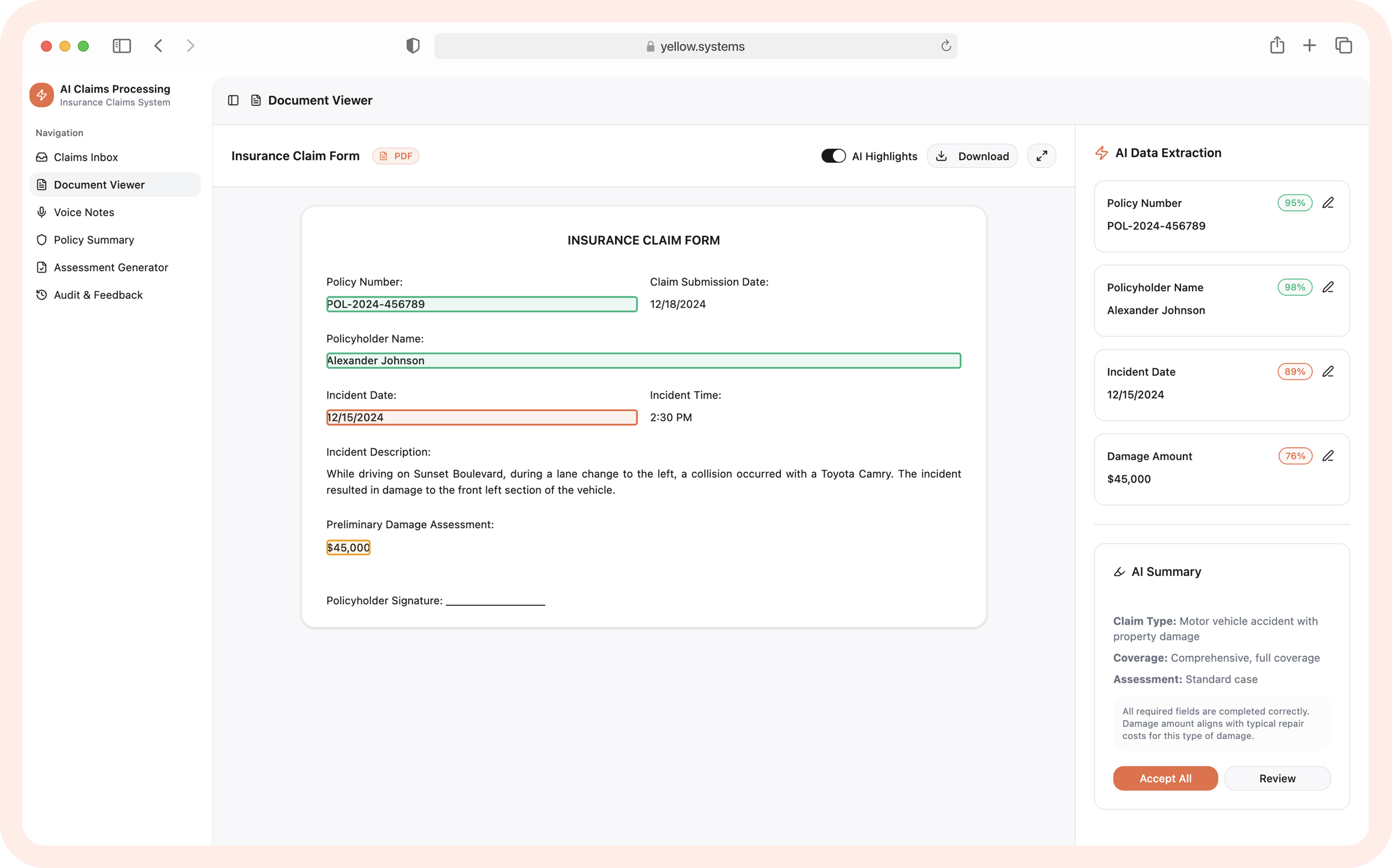
Web UI for review/editing of AI-generated claim drafts
Data security measures and compliance with insurance data standards
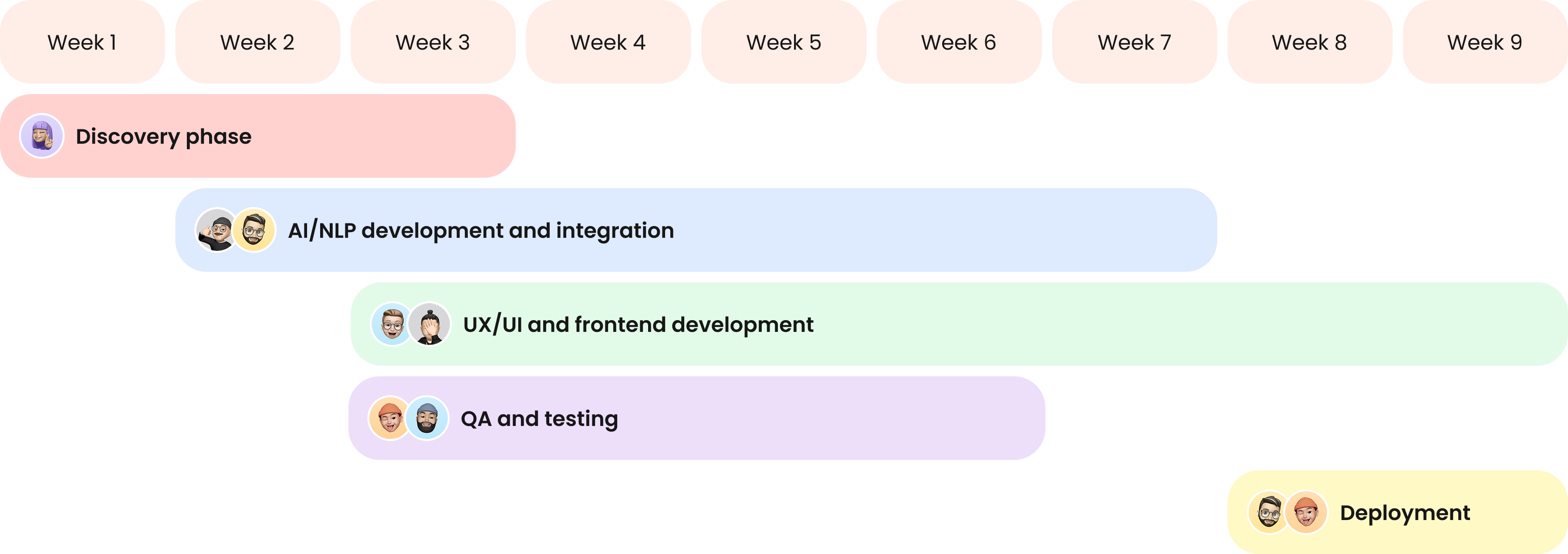
Project timeline
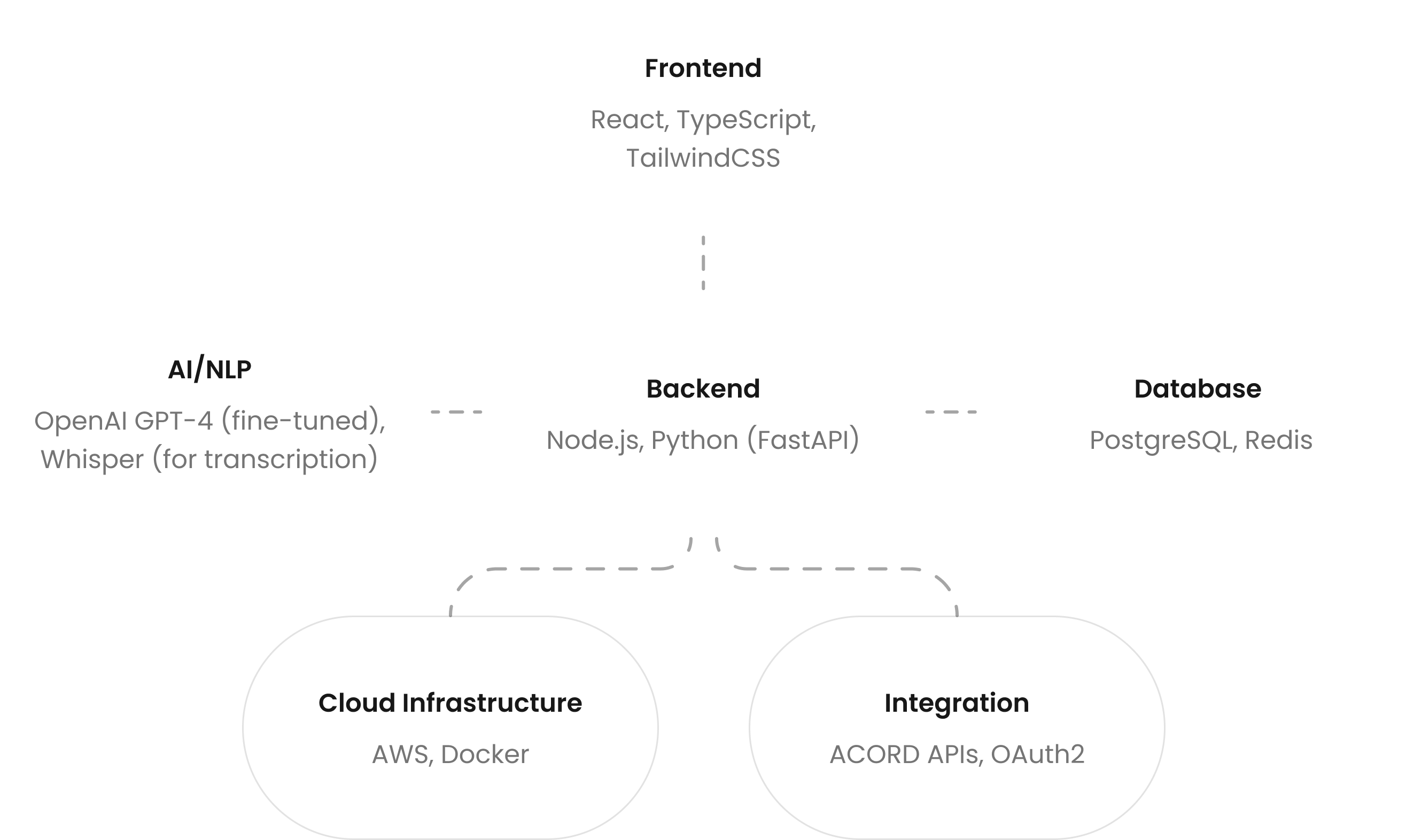
Tech stack
The technologies we used to realise the LLM integration smoothly.
Development challenges and solutions
How our team dealt with a range of development challenges.
Accurate transcription of claim interviews
Challenge: Insurance claim interviews often involve poor audio quality, with a lot of background noise and overlapping voices. Standard transcription models struggle with domain-specific vocabulary, and out-of-the-box solutions frequently misinterpret critical phrases.
Solution: We fine-tuned Whisper with call center audio samples and enriched the output using domain-specific insurance terms. This customization allowed the system to adapt to noisy conditions and speech patterns. The result was more precise transcriptions that reduced the need for manual correction and editing.
Reliable claim summary generation
Challenge: While AI-generated summaries helped speed up claims review, early AI outputs were too generic or included irrelevant details, especially for complex multi-party claims. This created a risk of misinterpretation and slowed decision-making.
Solution: We used structured prompts that enforced policy-aware summarization and added confidence scoring. This approach reduced manual review time, improved accuracy, and provided users with clear and actionable summaries.
Result
By combining LLM-powered AI with deep insurance domain adaptation, we streamlined one of the most repetitive parts of the claims process. The resulting automation now plays a central role in reducing manual overhead for claims adjusters and speeding up case turnaround time.